Contacts for Glaucoma Detection
Glaucoma is a primary cause of vision loss and blindness in the US. While severe glaucoma-related vision loss can often be prevented, there is one major barrier: around half of patients with the disease do not know they have it. Glaucoma can take away as much as 40% of a person’s sight without them realizing. Once the vision is gone, it cannot come back.
Glaucoma is a group of conditions that cause damage to the eye’s optic nerve – a cluster of more than a million nerve fibers. The optic nerve links the retina – the light-sensitive layer at the back of the eye – to the brain; any damage to the optic nerve can lead to vision loss and blindness. Early diagnosis, however, opens the door to a number of treatment options that can halt glaucoma-related vision loss.
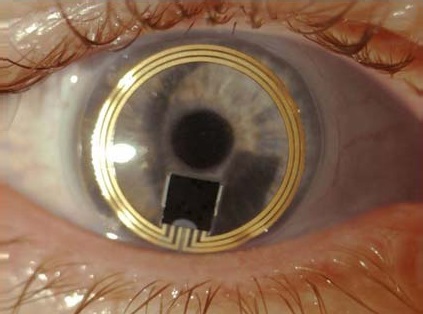
Early glaucoma treatment can be successful if the symptom of elevated pressure is under control. It has long been recognized that, since intraocular pressure varies during the day, continuous monitoring of glaucoma patients is needed. The static measurements currently performed during office hours are not able to detect pressure peak variations especially at night while sleeping. Monitoring gauges embedded into a silicone contact lens measures fluctuations in intraocular pressure. The patient wears the contact lens for up to 24 hours and undertakes normal activities including sleep periods. When the patient returns to his doctor, the data is transferred from the recorder to the practitioner’s computer via Bluetooth technology for immediate analysis. Findings clearly demonstrate that IOP reduction is beneficial in decreasing progression of glaucoma, although treatment does not necessarily prevent disease advancement.
During a general eye examination IOP measurements are taken every year. Although IOP is not a single value it fluctuates similarly as does blood pressure.
These contact lens devices that monitor IOP continuously have shown that there is a circadian rhythm to IOP. IOP is generally highest (by roughly 5mm Hg) during the night compared with daytime levels. IOP also exhibits significant minute-to-minute and day-to-day fluctuations not readily apparent in periodic IOP measurements obtained by standard tonometry. IOP fluctuation may be a strong risk factor on its own for the risk of disease progression in glaucoma patients, independent from mean IOP levels. The Advanced Glaucoma Intervention Study supported IOP fluctuation as a significant risk factor for glaucoma progression leading to the need to monitor IOP in at risk individuals through a 24 hour period. Besides contributing to our overall understanding of IOP fluctuations in glaucoma patients, this data could be used to ensure that a more appropriate target IOP level is chosen for each patient. Specifically, a lower target mean IOP might be set for a patient in which IOP variability is greater, resulting in more individualized therapeutic regimens. Information could be sent electronically to the doctors office on a regular basis, alerting the clinician to periods in between appointments when the IOP stays above the desired target range. In these instances, the clinician can proactively alter the treatment.
Diabetes is another pathology that innovations will help many patients by wearing a glucose sensing contact lens. Diabetes is a growing problem affecting one in every 19 people on the planet. These patients struggle daily trying to keep their blood sugar levels under control. Uncontrolled blood sugar puts people at risk for a range of dangerous complications, some short-term and others longer term, including damage to the eyes , kidneys, legs and heart.
Although some people wear glucose monitors with a glucose sensor embedded under their skin, all people with diabetes must still prick their fingers and test drops of blood throughout the day. It’s disruptive, and it’s painful. And, as a result, many people with diabetes check their blood glucose less often than they should.
On the horizon will help many patients with diabetes by wearing glucose-sensing contact lens. The system would likely contain the contact lens itself, which would sense glucose levels; and a “reader” device, which would communicate and power the contact lens. A user display, would allow patients to see and review their blood sugar data and help stabilize their blood sugar during the day.
Research has shown that maintaining blood glucose levels within an acceptable range can lower and delay risk for complications. The current acceptable blood glucose target ranges set by the American Diabetes Association (ADA) are as follows:
- Fasting/pre-meal: between 70 and 130 mg/dL
- One to two hours after meal: below 180 mg/dL
It is important to remember that the purpose of your blood glucose readings is to let you know how close you are to your target range.
